In an effort to better understand the mechanisms that contribute to injury and to design better programs to make our players more durable on the ice, I’ve read a ton of research on hip injuries, such as hip flexor/adductor tears, sports hernias, osteitis pubis, femoroacetabular impingement (FAI), and labral tears over the last several years. While I recognize that every injury is multi-factorial, I always frame injuries within the context of “what can we do to minimize risk, if not prevent them?”
It’s become clear along this journey that hip injuries tend to coincide with one another and the issue is almost always much more complex than simply “overuse” or “we found a labral tear, which needs to be repaired.” This latter point was highlighted by a 2011 study from Silvis et al. that demonstrated that 77% of the 39 NCAA D1 and pro hockey players had abnormal hip/groin MRI findings that were indicative of pathology, despite being entirely asymptomatic (Read the abstract here: High prevalence of pelvic and hip magnetic resonance imaging findings in asymptomatic collegiate and professional hockey players). This is a hockey-specific example, but there are others looking at different joints and in different populations that support the idea that something appearing broken may not always lead to pain and may not always need to be repaired.
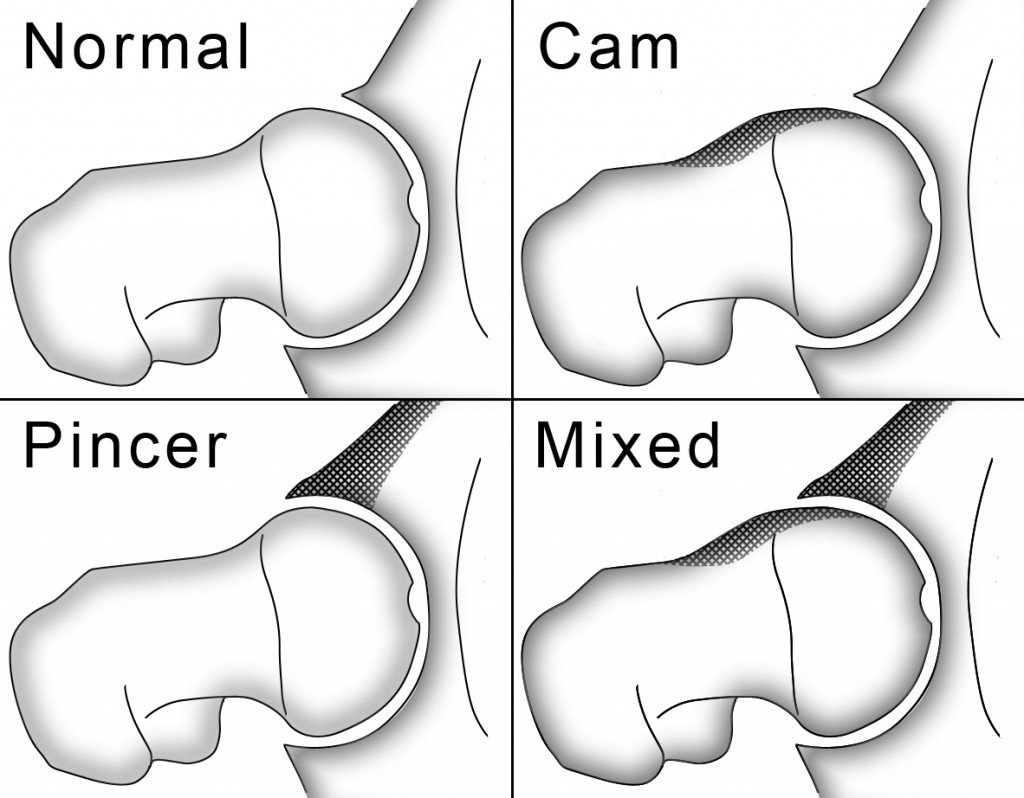
When I first started to read about how FAI (a bony overgrowth of either the femoral head/neck offset and/or the acetabular hood; image below) limited hip flexion ROM, I began including some assessments in our intake to help screen for those limitations and, over time, developed a better eye for seeing suspicious compensations throughout various exercises. Despite there not being clear research evidence in support of FAI being developmental (there was a thought that it was congenital and/or developed from a slipped capital epiphysis, both of which are explanations I believe hold merit in a minority of cases), I never really had any doubt that the majority of these cases are progressive, likely resulting from poor femoral head tracking and too much time or volume spent at or near end-range hip flexion. This is important, because if things are progressive there is an opportunity to intervene. Given that this bony overgrowth is associated with increased anterior-superior labral wear/tearing and eventual osteoarthritis (see Streit et al, 2013, among others), the need be proactive in minimizing risk is important from both a short- and long-term perspective.
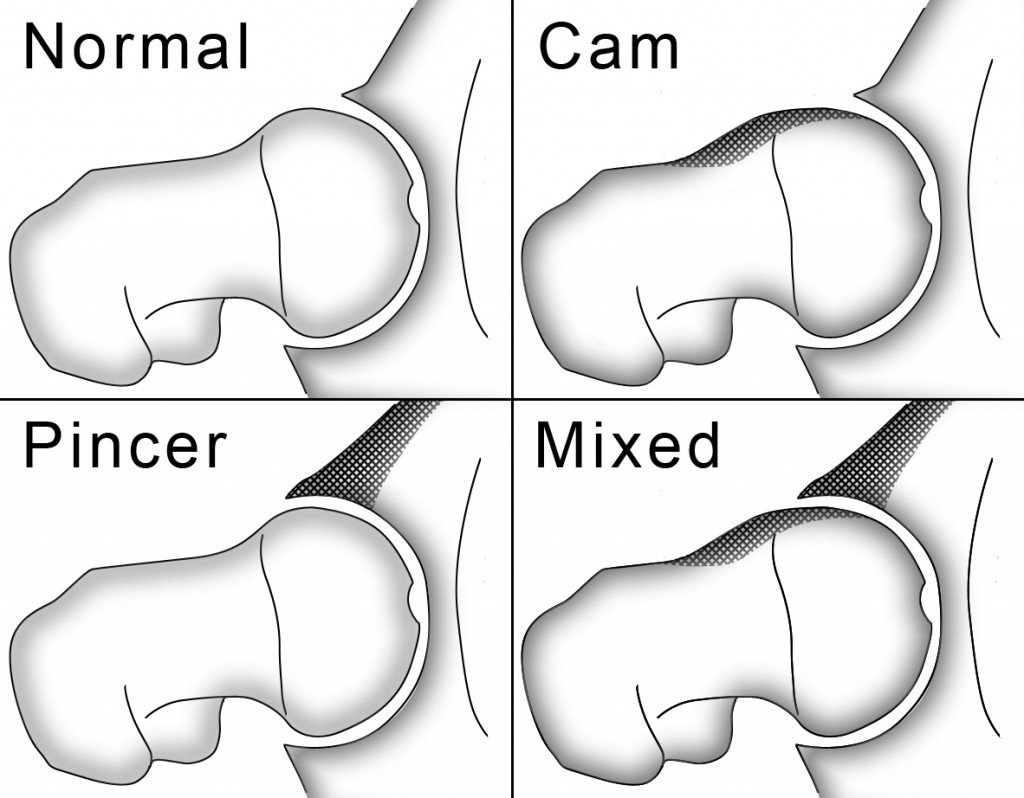
A demonstration of the bony overgrowth illustrative of FAI
In the last few months, several interesting articles have been published that continue to shed light on this issue. First, Larson et al. (2013) published data on NFL prospects in college and found that 90% of the 125 athletes they looked at and 87% of the hips (an alarming statistic!) had findings consistent with FAI. Of these players, those with symptoms tended to have a greater prevalence of CAM or Mixed FAI and osteitis pubis, but the only independent predictor of groin pain was how progressive the bony overgrowth was (the “alpha angle”). This is interesting for a few different reasons. As I mentioned in the past (See: An Updated Look at Femoroacetabular Impingement), hockey players aren’t the only population affected by this hip “abnormality”. This is the first study I’ve seen (admittedly, I’m not looking for other sports) that has used an athletic population not typically put in the most “at risk for hip injury” bucket. As a backdrop, it suggests that as the bony overgrowth gets worse, the athlete is more likely to be symptomatic.
This latter fact is not surprising given a 2012 study from Birmingham et al. that concluded:
“Dynamic femoroacetabular impingement as caused by the presence of a cam lesion causes internal rotation motion at the pubic symphysis. Repetitive loading of the symphysis by cam impingement is thought to lead to increased symphyseal motion, which is one possible precursor to athletic pubalgia.”
As a follow up, increased motion at the pubic symphysis is also a risk factor for osteitis pubis (inflammation in the area), which is another cause of groin pain.
So what does this have to do with hockey players? I’ll get there!
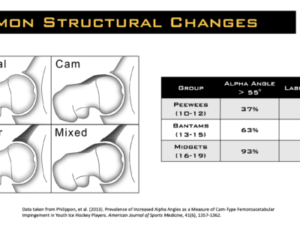
A study published last month from Philippon et al. provided solid evidence that FAI is in fact developmental/progressive, at least in the hockey population. In short, they imaged the hips of 61 youth hockey players from 10-18 years old, and found that:
- In PeeWees (10-12 y/o), 37% had FAI and 48% had labral tears
- In Bantams (13-15 y/o), 63% had FAI and 63% had labral tears
- In Midgets (16-19 y/o), 93% had FAI and 93% had labral tears
While there will inevitably need to be follow up studies done, this provides some interesting information as to how these structures develop, and really highlights how important it is for hockey coaches, strength and conditioning coaches, and sports medicine professionals to be aware of their existence. In short, a player may not be skating lower because he/she physically does not possess the structure to achieve a deeper stance (remember this is a BONY block; it can’t be stretched), and he/she may not be able to squat/lunge/deadlift like textbooks suggest they should be able to for the same reason.
While slightly tangential to the previous conversation, a 2013 study from Jakoi et al. found that NHL players were less productive in the 2 years following sports hernia surgery than they were prior to the surgery. This was especially true for the “veteran” group (7 or more years in the league) as they played significantly less games per season (from 70.5 to 49.0), scored less goals per season (17.1 to 7.8), had less assists (25.4 to 13.1), and weren’t able to play as much time per game (from 18.6 to 15.2 minutes). While the declines in games played, goals and assists weren’t significant for the younger group (6 or less years in the league) there was still a decline despite playing more minutes per game (from 16.4 up to 18.4). When you factor in the total minutes played per season (games played x minutes per night), the younger group had almost equivalent minutes pre- and post- surgery (1077.48 vs. 1074.56), but still averaged less goals and assists following the surgery. This certainly isn’t to dismiss the potential benefits, and in some cases the necessity of the surgery, but instead should be taken as another argument for the importance of recognizing risk factors and intervening early.
There is a theme to this discussion. While it may not be possible to PREVENT 100% of injuries, it is important to do whatever is possible to screen/assess for risk factors, provide corrective strategies when appropriate, and coach around limitations that do exist so as to not exacerbate the problem. Given the data on how prevalent structural abnormalities are in athletes in a variety of sports, as well as the short- AND long-term implications of these injuries, taking the appropriate steps to improve an athlete’s durability may not just change your season (the two goal decrease in production could be the difference between making the playoffs or not, winning the championship or not), it may change his/her life.
Over the last several years, I’ve gotten a lot of questions about how I assess our players, what I’m finding, and how this influences my programming. In my new DVD Optimizing Movement, I cover these very topics in detail. For the first time ever, I discuss the exact assessment protocol I use (including videos of the assessments), how we integrate corrective strategies into group settings (and how you can too), how we alter exercise selection based on assessment findings, and the 4 things that underlie correctly performing almost every exercise. The DVD has gotten outstanding feedback from everyone ranging from personal trainers, to sports med professions in professional sports, to collegiate strength and conditioning coaches, to private physical therapists. Check it out at the link below!
Click here for more information and to watch the trailer! >> Optimizing Movement
To your success,
Kevin Neeld
UltimateHockeyTraining.com
References:
- Silvis, et al. (2011). High Prevalence of pelvic and hip magnetic resonance imaging findings in asymptomatic collegiate and professional hockey players. American Journal of Sports Medicine, 39(4), 715-721.
- Streit, et al. (2013). The shape of the proximal femur influences acetabular wear patterns over time. Clinical Orthopaedics and Related Research, 471(2), 478-485.
- Larson, et al. (2013). Increasing alpha angle is predictive of athletic-related “hip” and “groin” pain in collegiate national football league prospects. Arthroscopy, 29(3), 405-410.
- Birmingham, et al. (2012). The effect of dynamic femoroacetabular impingement on pubic symphysis motion: a cadaveric study. American Journal of Sports Medicine, 40(5), 1113-1118.
- Philippon, et al. (2013). Prevalence of increased alpha angles as a measure of cam-type femoroacetabular impingement in youth ice hockey players. American Journal of Sports Medicine, 41(6), 1357-1362.
- Jakoi, et al. (2013). Sports hernia in National Hockey League players: does surgery affect performance? American Journal of Sports Medicine, 41(1), 107-110.
Please enter your first name and email below to sign up for my FREE Athletic Development and Hockey Training Newsletter!





 Use CODE: "Neeld15" to save 15%
Use CODE: "Neeld15" to save 15%