Concussions have been a hot topic over the last two years in the NHL. Not in small part to Sidney Crosby’s concussion, more attention is now being paid awareness, prevention, and more conservative return-to-play guidelines.

Long-term concussion symptoms are becoming a more prevalent problem
Concussions are far from a simple injury. It’s the underlying complexities in injury mechanism AND predisposition that makes concussions so hard to treat. As I’ve mentioned in the past (see Sidney Crosby’s Concussion), a large component of preventing things from getting worse than they need to is following a complete return-to-play sequence. Given the alarming statistic that 92% of repeat-concussions occur within 10-days of the original incident, it would seem logical that a bare minimum precaution should be to keep players out for 2 weeks following ANY concussion suspicion. I can see the hesitation in adopting this practice as a norm, but the reality is that the amount of development and exposure that can occur within this time frame is negligible, especially when put in the light of the potential short- and long-term consequences of suffering a repeat head injury.
As my friend Maria Mountain recently wrote (see A Rant about Concussions in Hockey), it’s bizarre that the phrase “concussion-like symptoms” seems to frequent hockey media channels now. This is a suspicious description given both the diverse nature of concussion symptoms (which can range from those comparable to tension headaches to those resembling vertigo), and the lack of clarity in diagnosis in general. How does someone suffering concussion-like symptoms differ from someone with a concussion? Is concussion-like symptoms simply being used as an umbrella diagnosis to put a name on something not medically understood? If concussion-like symptoms are being used as a diagnosis for those exhibiting symptoms that don’t present with observable brain trauma and/or have relatively normal ImPACT scores, then it’s important to look at some of the underlying mechanisms that dispose athletes to these symptoms. There are certainly a lot of questions that remain to be answered regarding concussions, but with the increased attention being paid to the associated consequences of impact and adaptations to the brain itself, I thought it would be beneficial to discuss some of the lesser known underlying causes of “concussion-like symptoms” that may be related to or exacerbated by impact, but aren’t necessarily a brain injury.
Mechanisms of Concussion-Like Symptoms
Below are three mechanisms that can cause concussion-like symptoms, that are not associated with a brain injury:
Poor Visual Tracking
I was first introduced to this idea by Dr. Josh Bloom at Pete Friesen’s Physio-Fitness Summit a couple years ago. Dr. Bloom pointed out that in players with ongoing symptoms, or those that do not seem to be making progress, it is often the case that they have an eye that is not tracking properly. In a sort of ocular constraint-induced movement therapy, the employed strategy involved covering the properly functioning eye and training the eye that did not track optimally. He noted that in some cases, symptoms resolved almost immediately (within a single session) and had no recurrence. Whether ever player has this experience or not, it’s certainly worth looking into. The idea that a player may have ongoing symptoms that they think are related to a concussion may cause inappropriate limitations in their training and practice and a delayed return to play.
Sub-Occipital Nerve Impingement
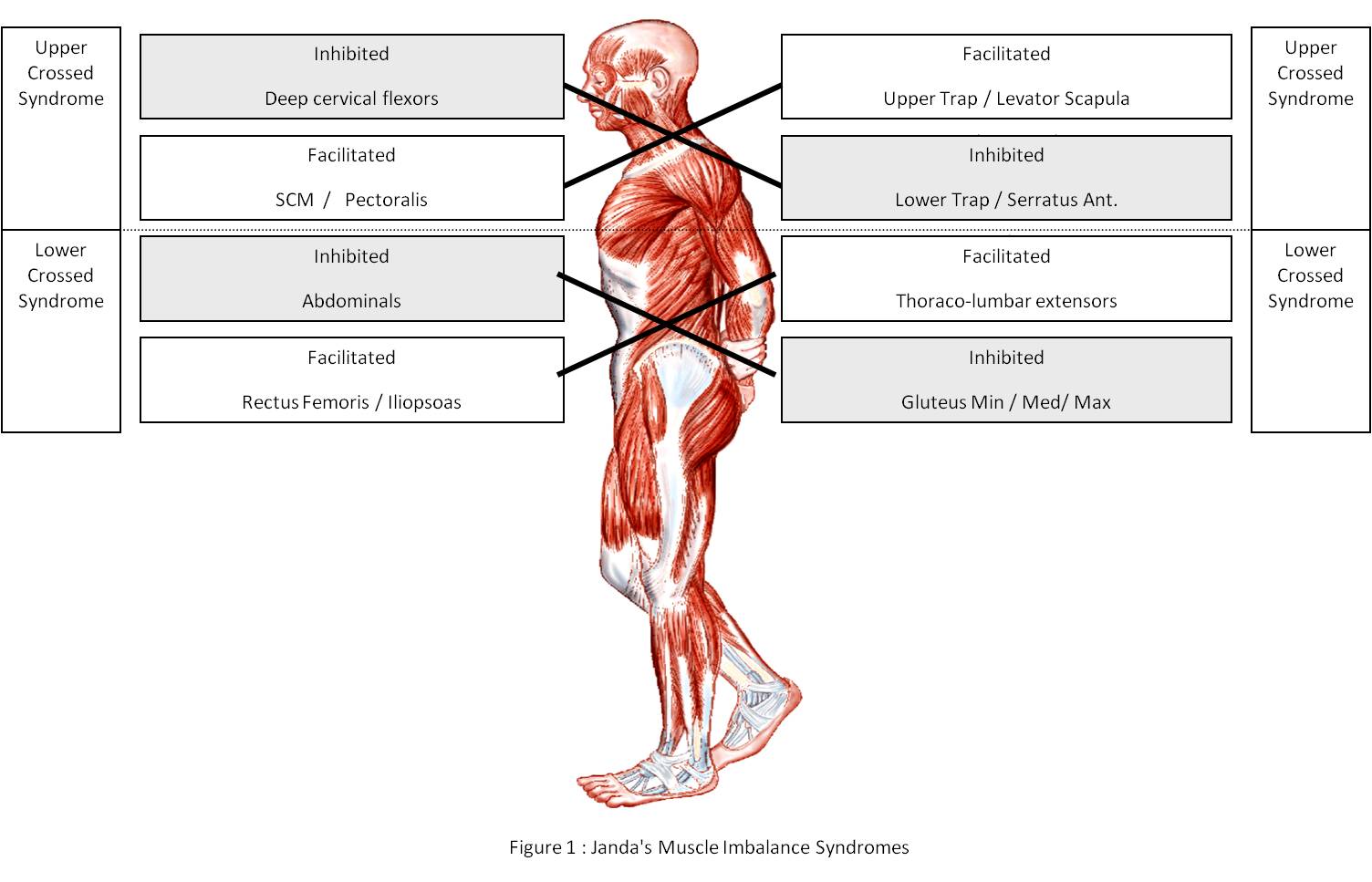
Over the Summer, my friend Ned Lenny (physical therapist based in Cherry Hill, NJ if you’re local) and I were talking about postural adaptations that we see in both the hockey and general populations, and about how the hockey adaptations were typically in-line with a more extreme version of what we saw in the general population. In other words, the postural changes we see in most people that result from sitting too much and moving too little are significantly worse in hockey players. In general, these adaptations can be described by Janda’s upper and lower crossed syndromes.
Ned pointed out that hockey players spend a substantial amount of time sitting on the bench, in cars/buses/airplanes, playing video games at home, and after many practices and games, they hop on a stationary bike. Going for a post-skating bike ride isn’t inherently harmful; in fact there is some value in restoring a more optimal autonomic nervous system balance. The kicker is that players hop on the bike and immediately look for the TV, which is usually posted above their heads somewhere, forcing them to rotate their head further back. Living in this position of posterior cranial rotation predisposes them to suffering symptoms related to impingement of the local nerves when forced further into posterior rotation, which can result from contact of varying severity. This might be why you see some players with prolonged symptoms after taking what looked like a relatively innocent hit.
The key to minimizing this predisposition is to improve the player’s posture and awareness of cervical position. We spent a lot of time last off-season emphasizing a “packed neck” position with all our hockey players at Endeavor and continue to emphasize this position now with our in-season groups. In reality, this isn’t an injury prevention strategy as much as it’s just the right way to train, but it can feel a bit unnatural for players at first.

Chicks dig guys with a good neck pack
Altered Sensory Input Secondary to a Loss of Neutrality
This is a very complex way of saying that humans are inherently asymmetrical and have tendencies to drift toward predictable positions of non-neutrality. This concept stems from my ongoing apprenticeship of the Postural Restoration Institute information, and has profound implications for athletes and non-athletes alike. Over the last week at Endeavor, I’ve assessed a dozen people that all had NO adduction on their left side, but had full adduction on their right side. For hockey players, this pattern will compromise their stability and skating power, and it’s likely that a player will feel more comfortable crossing over one way (usually to the right) than the other. Failing to address this pattern can lead to a number of compensations of varying severity. Luckily, neutrality can be restored pretty easily using a number of specific breathing techniques.
Importantly, these human tendencies aren’t limited to the hips, but affect everything from the position of the foot to the position of the temporal bones. Specific to the cranial region, it’s worth noting that the common adaptations in the spine lead to a non-neutral head orientation. Because the body naturally seeks a position where the eyes are horizontal, there are compensations that occur through the spine, bones of the head, and the ocular system, all of which will alter the related sensory input, and can lead to feelings of dizziness or general feelings of spatial instability. I realize this is an abstract concept, but it’s not one to be overlooked. At PRI’s Advanced Integration course a couple weeks back, Ron Hruska discussed what he referred to as “ocular scoliosis” and noted that restoring neutrality can actually change a person’s eye prescription. The eyes are among the body’s most powerful sensory organs. Restoring a more neutral position can lead changes in sensory “symptoms” stemming from multiple sources.
Take Home
The major take home from this discussion is that it’s possible to have symptoms resulting from contact that resemble those of a concussion that have an underlying cause not related to brain impact. Because all of the above mechanisms have relatively quick fixes, they’re certainly worth exploring if you have ongoing symptoms AND should be attended to regularly in the interest of minimizing concussion risk in the first place. With the medical team that Sidney Crosby has put together, you would hope that these, and all other underlying factors, are also being addressed.
That’s a wrap for today. Pass this along to other players, parents, and coaches, or anyone else you think may benefit from learning more about concussion prevention!
To your success,
Kevin Neeld
Please enter your first name and email below to sign up for my FREE Athletic Development and Hockey Training Newsletter!